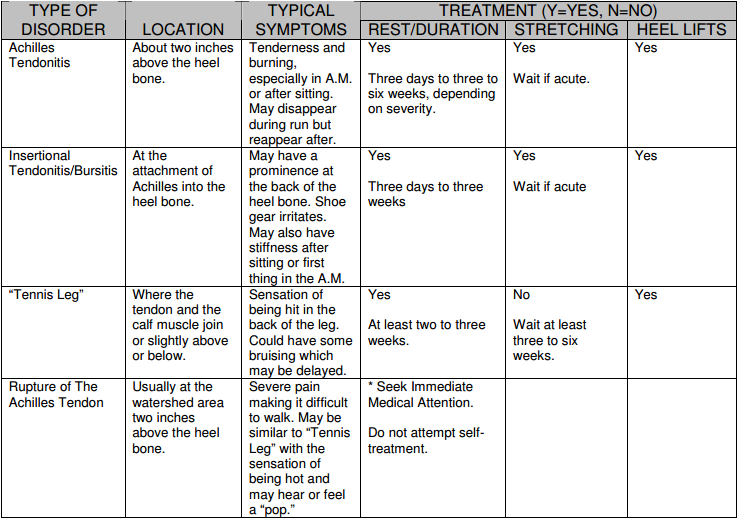
Last month, we looked at Achilles tendon disorders from the standpoint of the anatomy of this area and how different forms of these disorders tend to manifest themselves in the forms of symptoms.
This article is going to focus on some self treatment you can try on your own as well as some
alternative forms of treatment your sports medicine specialist may recommend.
Self -Treatment
When it comes to self treatment, many times the same form of treatment may or may not be
beneficial depending on the form of Achilles disorder you have.
At the end of the article, I will summarize the different forms of treatment, whether it may be beneficial
for your type of problem and when you may want to start. These are not hard and fast rules, but can provide an outline for you.
One constant with many forms of self treatment may be some period of rest. One can always
supplement your period of non-running with swimming or water running to help maintain your fitness as well as your sanity.
A. Achilles Tendonitis
Once again, as discussed in last months article, this form of Achilles tendon injury usually occurs
about two inches above the heel bone. You may find swelling when compared to the other leg in the
same region. Because of the poor blood supply to the area, it is important to initiate treatment
immediately to prevent the tendonitis from becoming chronic.
Evaluate the area
With your thumb and forefinger, pinch along the Achilles tendon. Start down close to the heel,
working your way up toward where the tendon enters the calf muscle. If you feel swelling and
pain, you likely have Achilles tendonitis.
Early Treatment
Stop running. (This is where you rip out this page and throw it in the trash, right?) I recommend taking at least two to three days off completely. During this time you should ice the area 15-20 minutes two to three times a day. Use ice packs or massage the area with a Styrofoam or Dixie cup filled with water and frozen, peeling off the top layer of paper as you go. Do not stretch the area during this initial period because you only serve to keep the area inflamed and may risk further damaging the
area.
Next, use heel lifts to take the stress off the Achilles. Use a ¼ inch non-compressible material. In your running shoes I recommend placing the lift under your existing insoles. I have found the following to work well; take the insoles from a couple pairs of old running shoes and cut straight across about three inches from the back of the insole. Two layers will be about ¼ inch. Two layers will be about ¼ inch. You can use any other non-compressible material you have around the house. Be sure to do this on the non-affected leg as well, otherwise you will be creating an imbalance which may result in further injuries. It is important not to walk around without your shoes, even in the house (except when taking a bath or
shower). The farther the heel must go to reach the ground, the greater stretch and re-irritation of the Achilles.
If you return to running and have no significant pain or alteration of running gait, do no speedwork or hillwork for at least three weeks. If you return to running but continue to have pain such that it causes you to alter your normal running gait, then your better off not running. If you continue to have pain despite time off, ice and heel lifts, then it is best to seek a sports medicine physicianfor a more thorough evaluation.
Possible Medical Options
Treatment may include physical therapy, non-steroidal anti-inflammatory medications (NSAID’s),
massage therapy, night splints and possible cast immobilization. If biomechanical abnormalities are present such as overpronation, leg length differences or other pathology is present, orthotics may be required. Also, an MRI may be recommended to further evaluate the extent of damage and
possible tears. Surgery may be considered as a last option.
B. Insertional Achilles Tendonitis/Bursitis
This injury occurs where the tendon inserts into the heel bone instead of above it. Chronic irritationcan, at times, cause a spur to develop within the tendon itself. This condition can also result in an inflammation of a small fluid-filled sac in the area called the retrocalcaneal bursa.
Evaluate the area
Push the area on the back of the heel. You may notice a thickening in this area as well as
tenderness. There is a similar problem to the achilles insertional spur which also causes an
enlargement on the back of the heel called a haglund’s deformity or “pump bump”. This can only be differentiated from insertional Achilles tendon spur by x-rays and careful examination. The
conservative treatment for the haglund’s deformity is similar to a Achilles insertional spur so, for the sake of length this article, we won’t go into a lot of specifics on how these problems differ.
Self – Treatment
Be sure the back of your current running shoes are not so worn that there is a hole in the area behind your heel. Next, find something to cushion the back of the heel (such as adhesive felt or foam) and cut a doughnut or U-shaped pad so that the area of irritation sits inside the “doughnut hole” or “U”. Place this in the back of the shoe so the pressure is off the irritated area. You can also try multiple layers of moleskin or cut a “U” in the back of a heel cup.
Ladies, stay away from “pumps” and high-heeled shoes that may aggravate the area. Try clogs or
sandals whose strap does not come across this area.
Possible Medical Options
Be sure your current running shoes are not too worn out and you are using the correct type for
your running biomechanics. Treatment is very similar to that of standard Achilles tendonitis so review that area again. I’ll frequently use different custom forms of padding and be sure my patients are not just performing the standard “calf” stretch but also the “soleus” stretch in which the back leg has the knee bent instead of straight to localize the area of pain more effectively. Once again, surgery should only be considered as a last option. A new option that may be available in the future is shock wave therapy or ESWT (extracoporeal shock wave therapy). This technology uses deep shock waves to break up scar tissue and allow new vessels to flow into the area to help the Achilles tendon insertion heal itself. This is still in the investigational stages with pending FDA approval for insertional Achilles tendonitis, but it does show promise. This is the same technology being used in chronic plantar fasciitis.
C. “Tennis Leg”
This injury occurs at the junction of the calf muscle and the Achilles tendon or just below this area.
Evaluate the area
As mentioned in the last article, you may have the sensation of being hit in the back of the calf and possible bruising. Pain and swelling may even extend into the ankle area. This usually occurs as a result of more ballistic movement such as reaching for a tennis shot (hence the name “tennis leg”) or from trauma. My two incidents with this injury occurred while playing basketball and doing intervals on the track. Pushing at the junction of the bottom of the calf muscle and thinner Achilles tendon will illicit symptoms as noted above.
Self – Treatment
Initially includes RICE: rest, ice, compression and elevation. Your sports medicine physician should
evaluate this problem to ascertain if the Achilles tendon has been torn. Do not run until the injury has been evaluated.
Possible Medical Options
Usually this requires no running for at least two to three weeks. Physical therapy, message therapy
and gradual stretching can speed the healing process. Once again, heel lifts in both shoes will likely
be of benefit and anti-inflammatories may be prescribed. Also, no speedwork or hillwork is allowed; typically at least six weeks or until pain has subsided.
D. Achilles Tendon Ruptures
Rupture of the Achilles tendon, although not common, is a very serious injury and should be treated as such. As mentioned in last months article, the Achilles loses its elasticity from age 35 on and so it is more frequent in those of us in this group.
This is not a time to attempt self-treatment. Immediate evaluation by a sports medicine physician is essential, not only to help you return to running, but also to prevent further damage. Partial ruptures can usually be treated successfully with some type of immobilization such as a cast. Complete ruptures may require surgery.
PREVENTION
The easiest way to treat Achilles tendon injuries is to prevent them in the first place. These injuries can take several months to totally resolve and may result in the formation of scar issue and permanent limited mobility. With that in mind, it makes sense to take strides to prevent them. Keys to prevention include warming up sufficiently, maintaining appropriate flexibility, sensible running and wearing appropriate shoes.
Warming up includes starting all your runs at an easy pace. I always run the first 1-2 miles slowly,
usually 30 seconds to a minute slower than my normal training pace. This is especially true when
doing speedwork or hillwork. To help maintain flexibility, I feel stretching is in order. I know all you running gurus who read the
running literature these days will say the jury is still out on stretching and its proposed benefits. But from my own personal experience, I must say stretching has helped keep me on the roads, and my periodic bouts with Achilles injuries have usually been at times when I have not been stretching. If I do no other stretching, regardless of injury or not, I always try to stretch the Achilles. The simple straight leg and bent knee Achilles wall stretch performed gently for two repetitions each of 15-20 seconds has been my bread and butter. Also, I prefer to stretch after I’ve taken my one to two mile warm up so that I am not stressing an already tight region.
Sensible training includes allowing the muscles and tendons to adapt to increasing amounts of stress loads placed upon then. In regard to overall mileage and long run mileage, don’t increase more than 10% per week. In regard to speedwork or hillwork increase the speed, repetitions and distance gradually. And when increasing overall mileage per week or speedwork, only change one variable or the other at one time. Don’t increase both at the same time.
Wearing appropriate shoes is important. “Appropriate” refers not only to the correct type for your
running biomechanics, but also appropriate heel height. Many running specialty stores can evaluate
you and put you in the right shoe for your mechanics. Also, be aware that shoes having a lower heel, such as most racing flats or spikes, may put additional stress on the area because of the lower heel height. I have given up true racing flats and use lightweight training shoes with my orthotics to give me additional support, only using these for speedwork and races.
SUMMARY
As outlined in the previous paragraphs, the best way to treat Achilles tendonitis, or any injury for that matter, is to prevent it from happening. But as they say, “Even the best laid plans of mice and men sometimes go awry.”
When mild injuries occur, self treatment can be of benefit and keep you out of my office. But in the cases where the injury has not improved in a week despite the outlined measures or an Achilles tear or rupture is suspected, you need to seek the attention of the sports medicine physician.
See you on the roads!